NMOSD treatment
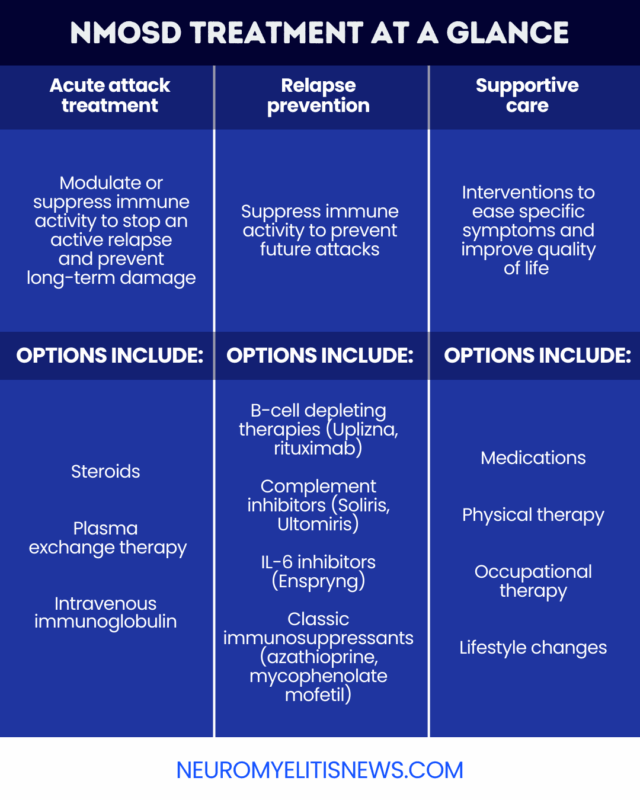
While there is no cure for neuromyelitis optica spectrum disorder (NMOSD), a rare autoimmune neurological disorder, NMOSD is treatable with medications to control active disease attacks, slow long-term disease progression, and manage symptoms.
In NMOSD, the immune system mistakenly launches inflammatory attacks on healthy parts of the nervous system, particularly the spinal cord and optic nerves, which drives disease symptoms.
An untreated NMOSD attack can cause irreversible nerve damage and contribute to long-term disability, so prompt treatment is important. The other cornerstone of NMOSD therapy is long-term maintenance treatment to reduce the risk of future attacks.
Treating acute NMOSD attacks
Most people with NMOSD experience a relapsing disease course, characterized by periods of suddenly worsening symptoms during which the immune system is actively attacking the nervous system.
Acute treatment should begin as soon as possible after an attack starts to prevent irreversible damage to the nervous system. NMOSD acute attack treatment may involve:
- steroids: intravenous (into-the-vein) or oral medications that reduce immune activity and inflammation
- plasma exchange, known as PLEX: a blood-filtering procedure that helps remove disease-causing antibodies and immune proteins from the blood
- intravenous immunoglobulin, or IVIG: antibodies from the blood of healthy donors, which are infused into the bloodstream to help normalize immune activity
High-dose steroids for NMOSD are the first-line approach for managing an NMOSD attack. These medications are typically given at a high dose for 3-5 days, and then slowly tapered off over several months.
PLEX treatment for NMOSD is used either as a second-line treatment for people who don’t respond well enough to steroids, or as a first-line treatment for people with severe symptoms or who have previously responded insufficiently to steroids.
IVIG for NMOSD attacks is not a standard approach, but may sometimes be used for patients who can’t receive other treatment options.
Long-term treatment to prevent relapses
Another major goal of NMOSD treatment is to prevent future relapses. After a first disease flare, most people with NMOSD will receive long-term maintenance therapies to slow disease progression.
In the U.S., there are four approved therapies that can be used for relapse prevention in NMOSD. Each works in a different way to block the immune activity that drives disease attacks:
- Enspryng (satralizumab-mwge): This subcutaneous, or under-the-skin, injection therapy is designed to block the activity of an immune protein called IL-6, which is believed to contribute to inflammation in NMOSD.
- Soliris (eculizumab): An intravenous therapy, this medication blocks the activation of a part of the immune system called the complement cascade that contributes to immune-mediated damage in NMOSD.
- Ultomiris (ravulizumab-cwvz): This is a successor to Soliris that works similarly but can be administered less often.
- Uplizna (inebilizumab-cdon): This intravenous treatment is designed to deplete B-cells, the immune cells that produce the harmful self-reactive antibodies that drive NMOSD.
All of these approved NMOSD medications are biologic treatments, meaning they contain components from living cells and organisms.
Each of the currently approved NMOSD therapies is cleared only for people who test positive for antibodies targeting the aquaporin-4 protein (AQP4), which are the most common type of disease-causing antibodies. There are no approved medications to date for NMOSD patients without anti-AQP4 antibodies.
Other immune-suppressing therapies are not officially approved for NMOSD, but are sometimes used off-label for NMOSD relapse prevention. These include:
- rituximab, an intravenous B-cell depleting therapy that is approved for NMOSD in Japan
- classic immunosuppressants, such as azathioprine or mycophenolate mofetil
For most people with NMOSD, immunosuppressive therapy is lifelong, although treatment may be discontinued in certain cases.
How doctors choose the right treatment
There is no one therapy that is universally considered best for all people with NMOSD. There are various factors to consider when choosing between NMOSD treatment options, including:
- disease type
- relapse history
- patient age
- NMOSD treatment side effects
- coexisting medical conditions
- treatment access and availability
- treatment cost
- frequency of infusions and mode of administration
Patients should work closely with their healthcare team after their NMOSD diagnosis to choose a treatment that will work best for them when all of these various factors are considered.
Monitoring treatment and managing side effects
Regular follow-up visits are key to monitoring treatment responses after starting a long-term NMOSD therapy. Clinicians may order laboratory tests and MRI scans to assess immune activity and monitor areas of damage.
Patients should always report any new or worsening NMOSD symptoms to their healthcare providers, as this can be indicative of a relapse.
Individuals should also let a healthcare provider know any time they experience new or unexpected side effects. NMOSD treatments suppress the immune system, which can leave patients vulnerable to serious infections. Patients should report signs of infection, such as sore throat, fever, or chills.
A doctor will also advise each patient on which vaccines are needed before starting treatment or during treatment, depending on the individual case. While most vaccines are still recommended, people receiving immunosuppressive therapy for NMOSD should not receive certain live vaccines.
Symptom management and supportive care
NMOSD management may also involve supportive therapies to help control symptoms, depending on each person’s needs.
- nerve pain: anti-inflammatory medications, antiepileptic medicines, some antidepressants, physical therapy
- spasticity: antiseizure medications, oral or injectable muscle relaxants, physical therapy
- bladder problems: physical therapy, lifestyle changes, standard medications for incontinence
- bowel problems: laxatives, stool softeners, dietary changes
- erectile dysfunction: standard erectile dysfunction medications
- fatigue: cognitive behavioral therapy, physical therapy
- depression: cognitive behavioral therapy, antidepressant medications
Neurorehabilitation therapy can help individuals with movement- and vision-related disability to experience a better quality of life. Such therapy combines physical and occupational therapy with targeted medications to help individuals regain function and independence when faced with disability due to nervous system damage.
What to expect after starting treatment
Living with NMOSD treatment will involve regular healthcare visits and careful monitoring.
There is no specific timeline for when an NMOSD therapy will start working. It varies broadly depending on specific medication being used and individual factors.
Doctors will usually run regular blood tests to see if the medication being used is suppressing immune activity. However, the main indication that a therapy is working is if it prevents new relapses over time.
Although NMOSD medications decrease the likelihood of relapse, even an effective one does not entirely eliminate the risk, and attacks are still possible.
If NMOSD attacks continue, symptoms worsen, or side effects become intolerable, a healthcare provider may recommend making adjustments or switching to a different medication.
Neuromyelitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 
