How discrimination in healthcare continues to affect NMO patients
Addressing the inequalities, prejudices that create barriers to treatment
Written by |
I sometimes joke that if I had served in the military, I’d win diversity bingo. As a minority woman with a disability, there are many boxes to check off on a self-disclosure form.
I am self-absorbed, though, and it’s time I do better.
Within the rare disease community, many patients have encountered discrimination or a lack of access to basic medical care. Living with neuromyelitis optica (NMO) is difficult enough without encountering prejudice, dealing with negative attitudes, or fighting to access treatment. No two NMO patients have the same path to diagnosis, and the way the disease first presents itself often varies.
As it turns out, we also experience differences in how we’re treated on this journey. The stories I’ve heard from my fellow patients about systemic inequality in healthcare shock me, break my heart, and anger me. It’s no joking matter that these problems not only persist in 2023, but seem further set into the fabric of our society.
Sexism in healthcare
When my NMO symptoms first appeared, my general practitioner ordered an MRI. Unfortunately, it only included my head, and not my spine. She was anticipating a multiple sclerosis diagnosis, which would likely appear as brain lesions.
After the MRI came back clean, my then-fiancé and I were told by another medical professional that “sometimes young women in their 20s look for ways to get attention.” We were disheartened.
Two months later, I suffered a transverse myelitis attack and was hospitalized.
It’s no secret that women are often treated like second-rate citizens, and it can even happen as we seek medical care. Many times I’ve been encouraged to bring my spouse to appointments. Healthcare professionals unconsciously speak to him right over my head as if I’m not present.
I wonder how same-sex couples are treated, especially since they are more likely to consist of women, as the U.S. Census Bureau reports. Plus, 80-90% of those with NMO are women and people assigned female at birth.
Racial inequalities in healthcare
I adore living in Toronto, Canada, because of its diverse population. You can be whoever you want to be. Toronto consists of several unique neighborhoods including Little India, Little Italy, Little Jamaica, and our infamous Chinatown. Unfortunately, the separation of these diverse communities also means that they can feel segregated.
As one might expect, patients are often directed to healthcare professionals close to their homes; however, not all medical centers or hospitals offer all specialties, like neurology, especially in disadvantaged neighborhoods.
This can mean delayed appointments and racial inequalities in how healthcare is accessed, even in a public system like ours in Canada.
Remote communities lack access
If there’s one positive that came from the pandemic, it’s that many of us learned how to function virtually. We can access healthcare, including checkups and prescription refills, from home. This has greatly benefited remote communities, especially those that are hours or even days from major metropolitan city centers. However, this doesn’t help patients who require more intensive medical care due to conditions like NMO.
Patients who reside in the northern parts of Canada, many of whom are members of the Indigenous community, must decide when to travel for medical care. Doing so can be quite costly, as these expenses aren’t covered by our public healthcare system.
If a financial burden stress cycle existed, it might look something like this:
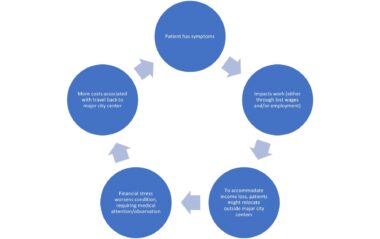
Financial burden stress cycle. (Infographic by Jennifer van Amerom)
The unpredictable nature of NMO can make it difficult to maintain a stable and reasonable income, creating a lot of stress and barriers to treatment for even the most advantaged patient.
Rare Disease Day
On Feb. 28, we recognize Rare Disease Day. It’s important to acknowledge patients who are already part of a small community; however, the day is also an opportunity to discuss the different types of discrimination that people battling rare diseases face. It’s time to acknowledge the prejudices that continue to create many unnecessary barriers for patients.
We each need to commit to speaking out about these injustices, and not just on Rare Disease Day. We need to petition our governments to make healthcare a human right, and not a privilege. And when faced with discrimination, even as a witness, we must call it out and stand against this behavior.
Note: Neuromyelitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Neuromyelitis News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to neuromyelitis optica spectrum disorder (NMOSD).





Leave a comment
Fill in the required fields to post. Your email address will not be published.