NMOSD overview
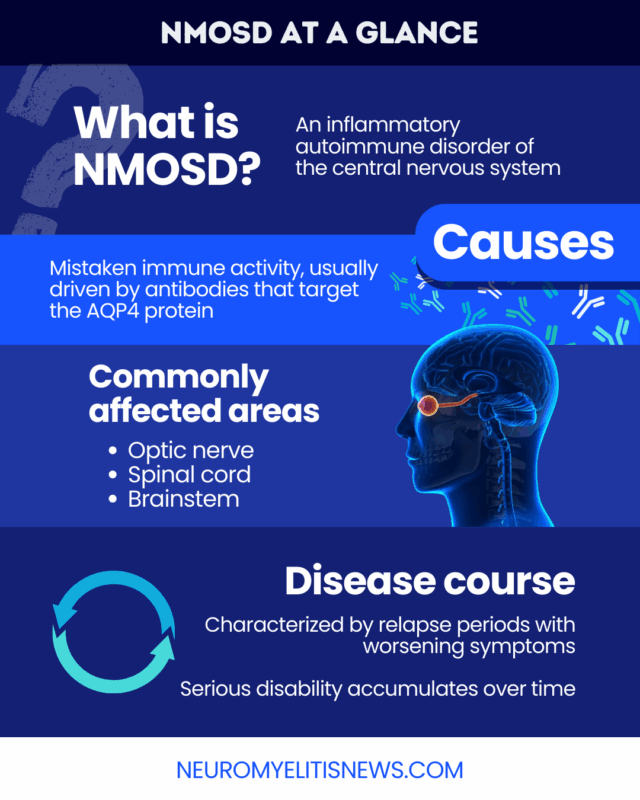
Neuromyelitis optica spectrum disorder (NMOSD), also called Devic disease, is an autoimmune disease that leads to inflammation and damage in the nervous system, causing symptoms such as vision problems, pain, and muscle weakness.
NMOSD is a rare condition, affecting approximately 1.5 people per 100,000 worldwide, and an estimated 22,000 individuals are living with the disease in the U.S.
There is no cure for NMOSD, but an early diagnosis and prompt treatment can help keep the disease under control, preventing or delaying serious disability.
What is NMOSD?
NMOSD is characterized by erroneous immune attacks that cause inflammation and damage in the nervous system, particularly in the spinal cord and optic nerves that carry visual signals between the brain and eyes.
The primary target of these attacks is a group of neural support cells called astrocytes, ultimately leading to nerve cell damage.
For most people, the disease is characterized by relapses, also called attacks or flares, which are periods when the immune system is actively attacking the nervous system, causing new or worsening symptoms. Each NMOSD relapse can cause irreversible damage, leading to progressively worsening disability over time.
Causes
The exact NMOSD causes are not entirely clear, and as with many other autoimmune conditions, scientists don’t know exactly why the immune system reacts the way it does.
About 70% to 80% of people with NMOSD have antibodies targeting the aquaporin-4 (AQP4) protein on astrocytes. These anti-AQP4 antibodies are thought to be key drivers of the immune activity that damages the nervous system.
In other cases, there are no detectable anti-AQP4 antibodies, and the exact cause of the disease remains unknown.
Other possible risk factors for NMOSD include:
- genetic factors
- history of other autoimmune conditions
- female sex and African or Asian ethnicity
- infections
- lifestyle factors, such as smoking or eating a high-sugar diet
Types
There are two main types of NMOSD, defined by whether an individual tests positive for AQP4-targeting antibodies.
AQP4 antibody-positive patients don’t need to meet as many clinical criteria to be diagnosed and have more treatment options. The minority of AQP4 antibody-negative patients, referred to as seronegative NMOSD, must meet more clinical criteria to be diagnosed and currently don’t have any approved treatment options.
Common symptoms
Most NMOSD symptoms are a consequence of inflammation and damage in the optic nerve (optic neuritis), the spinal cord (transverse myelitis), and, less commonly, in a brain region called the brainstem (brainstem syndromes).
Optic neuritis in NMOSD causes vision-related symptoms such as:
- eye pain
- blurry vision
- vision loss
The symptoms of transverse myelitis in NMOSD can vary, but may include:
- pain and other sensory changes
- muscle weakness, spasms, and other movement problems
- bladder and bowel problems
- sexual dysfunction
The most common brainstem syndrome is called area postrema syndrome, which can cause symptoms such as:
- uncontrollable hiccups
- nausea and vomiting
A range of other symptoms are also possible, depending on where the nervous system is damaged.
An NMOSD relapse can involve one or multiple groups of symptoms. The symptoms often develop suddenly, over several hours or days, and may persist for a few days or weeks. The length of time in between disease flares varies.
In the long term, NMOSD symptoms can cause severe and permanent disability, including blindness and paralysis requiring a wheelchair.
How NMOSD is different from MS
NMOSD is often confused with a more common autoimmune nervous system disease called multiple sclerosis (MS). Differentiating between NMOSD and MS can be challenging because they have many of the same characteristics. However, there are several key differences.
| Features | NMOSD | MS |
|---|---|---|
| Causes | Immune attacks target astrocytes; AQP4 antibodies are usually present | Immune attacks target myelin surrounding nerve cells; AQP4 antibodies are usually absent |
| Disease course | Almost always relapsing | May be relapsing or progressive |
| Relapse severity | Relapses are generally severe with poorer recovery; even a first relapse can lead to disability | Disease attacks are often less severe with better recovery; early relapses may not cause disability to worsen |
| Affected areas | Optic nerve, spinal cord, brainstem | Several areas of the brain are often affected, in addition to optic nerve and spinal cord |
| Symptoms | May affect both eyes at once
Cognitive problems are less common |
Usually affects one eye at a time
Cognitive problems are more common |
Blood tests and MRI scans can help clinicians distinguish NMOSD from MS. Proper diagnosis is vital because treatment approaches differ between the two conditions.
Diagnosis
Doctors often use a few different tests to diagnose NMOSD, including:
- physical and neurological examinations: assess NMOSD symptoms
- blood tests: identify disease-causing antibodies
- MRI scans: visualize inflammation and damage in the nervous system
- lumbar punctures: look for disease-related signs of immune activity and damage
Doctors will use findings from these tests to evaluate if a person meets the diagnostic criteria for NMOSD.
Establishing an NMOSD diagnosis requires ruling out other possible conditions, including MS and MOG antibody-associated disease (MOGAD), which have similar symptoms. An AQP4 antibody test and MRI findings can help make the distinction.
Reaching an early and accurate diagnosis is key for preventing irreversible nervous system damage. Working with a specialist who has expertise in how NMOSD is diagnosed can help ensure the right diagnosis.
Treatment options
NMOSD treatment has advanced significantly in recent decades, although there isn’t currently a cure. A therapeutic plan usually includes:
- acute relapse management
- long-term relapse prevention
- symptom management
A key aspect of NMOSD care is to immediately treat a relapse as soon as it starts in order to prevent irreversible damage. This may involve:
- oral or into-the-vein (intravenous) steroids
- plasma exchange therapy
- intravenous immunoglobulins
These work in different ways to stop the aberrant immune activity driving the attack.
After a first attack, most patients will start on long-term maintenance therapies to prevent future relapses. In the U.S., four therapies are approved for people with anti-AQP4 antibody-positive NMOSD:
- Enspryng (satralizumab-mwge)
- Soliris (eculizumab)
- Ultomiris (ravulizumab-cwvz)
- Uplizna (inebilizumab-cdon)
If these treatments don’t work or a patient has seronegative NMOSD, doctors may prescribe other therapies off-label, including classic immunosuppressants or rituximab.
Additional medications, alongside physical, occupational, and talk therapy, can also help ease specific disease symptoms and make daily life easier.
Outlook and long-term management
The specific NMOSD prognosis varies depending on the disease type, age of onset, location of damage, and other individual factors. Before effective treatments were available, around half of patients became wheelchair dependent and/or functionally blind after five years.
The early initiation of long-term relapse prevention therapies is crucial for improving the outlook for people with NMOSD.
Contemporary treatments can delay the onset of disability and have increased NMOSD life expectancy for most people. Without treatment, about 22% to 30% of NMOSD patients die within five years of diagnosis. Treatment reduces this mortality rate to 3% to 7%.
Living with NMOSD
NMOSD is a lifelong disease that can substantially impact a person’s everyday life. Living with NMOSD involves balancing symptom and medication management, healthcare visits, and daily activities.
Frequent communication and follow-up with a multidisciplinary care team is key. Patients should work with their doctors to develop a treatment plan that minimizes their risk of relapse and enables them to maintain the best possible quality of life.
Living with a chronic illness can also take an emotional toll. Patients and caregivers may benefit from mental health support, including counseling, therapy, or NMOSD-focused peer support groups to help them cope with the realities of NMOSD.
Neuromyelitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

