Analysis: Uplizna reduces number, size of subclinical spinal cord lesions
N-MOmentum analysis shows lesions were linked to future disease attacks
Uplizna (inebilizumab) reduces the number and size of subclinical lesions — those that cause no apparent symptoms — in the spinal cord of people with neuromyelitis optica spectrum disorder (NMOSD) about six months after the start of treatment.
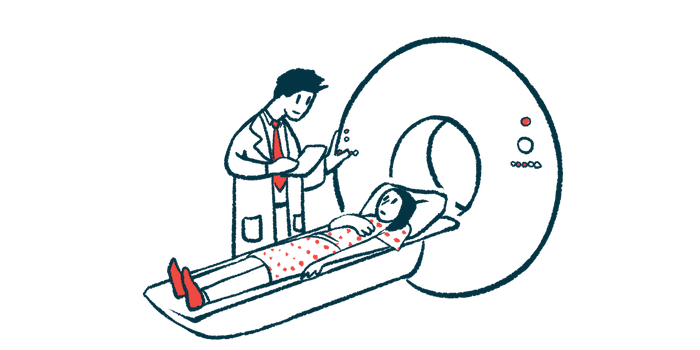
That’s according to a new analysis from the Phase 2/3 N-MOmentum trial (NCT02200770) that also showed these subclinical spinal lesions were linked to future disease attacks, suggesting they should be monitored over time by magnetic resonance imaging (MRI).
The findings add to a report of reductions in subclinical lesions in the optic nerves, which relay signals between the eyes and the brain, in Uplizna-treated patients in N-MOmentum.
The analysis “offers new insights into the significance of subclinical MRI findings on the spinal cord as a potential signal of future attacks, adding to the growing list of tools available for physicians to better monitor their patients,” Friedemann Paul, MD, the first author of the new analysis, said in a press release from Horizon Therapeutics, which markets Uplizna. “It is encouraging to see that Uplizna reduced the formation of these lesions. Future studies evaluating subclinical findings will help offer additional clarity on their relationship with disease activity.”
Paul is a group leader of the NeuroCure Clinical Research Centre at Charité-Universitätsmedizin Berlin, Germany. He presented the data in the poster “Characterization of Subclinical Spinal Cord and Optic Nerve MRI Lesions in the N-Momentum Trial” (abstract EPO-434) at this year’s European Academy of Neurology (EAN) congress, July 1-4 in Budapest, Hungary and virtually.
Changes in optic nerve, brain, spinal cord with Uplizna
NMOSD occurs when self-reactive antibodies — most often targeting a protein called AQP4 — react against healthy nervous system cells, causing inflammation mainly in the optic nerves and spinal cord.
Approved for adults with NMOSD who have anti-AQP4 antibodies, Uplizna works by promoting the death of B-cells, an immune cell type that produces antibodies. By doing this, it’s expected to prevent nervous system inflammation and ease disease symptoms.
In the N-Momentum trial, whose data supported the therapy’s approval, adults with AQP4-associated NMOSD were randomly assigned to receive either Uplizna or a placebo for six months. After that, they could enter an open-label extension phase where all were given the therapy for up to three years.
Administered directly into the bloodstream every six months after a loading dose, Uplizna was superior to a placebo at reducing attack rates and slowing disability progression, results showed.
During the trial, the researchers also used MRI data to look for changes in lesions, or areas of damage, in the optic nerves, the spinal cord, and the brain. Newly presented data concerned a posterior analysis of spinal cord and optic nerve inflammatory lesion activity data.
Of the 134 adults who completed the six-month placebo-controlled period without new symptoms, 20 (15%) had active lesions on the spinal cord and 65 (49%) had active lesions in the optic nerves. These lesions were classified as subclinical or asymptomatic because they didn’t cause any symptoms.
Compared with those detected around the time of an attack, the subclinical lesions were shorter. This was true with both the spinal cord and optic nerves.
Subclinical spinal lesions (both old and new) were less frequent, by nearly three times, in Uplizna-treated patients than in the placebo group, suggesting the therapy may reduce their formation.
Also, the frequency of new subclinical spinal cord and optic nerves lesions was reduced over time with continued Uplizna treatment in the study’s extension phase.
Linking lesions to attacks
Importantly, the presence of subclinical spinal cord lesions (either active or both old and new) was significantly linked to spinal cord-related NMOSD attacks in the year that followed. As such, by reducing subclinical lesions, Uplizna may help prevent future attacks.
“Attack prevention is a priority in managing NMOSD, as just one attack can lead to life-altering vision loss and mobility challenges,” said Kristina Patterson, MD, PhD, Horizon’s senior medical director of neuroimmunology medical affairs.
Moreover, significantly more patients with subclinical lesions in the spinal cord (but not in the optic nerves) had a twofold increase in the levels of the GFAP protein than those without lesions. GFAP is a marker of injury to astrocytes, the cells that are mainly attacked in NMOSD, and has been proposed as a marker of the disease’s activity.
Detecting subclinical lesions on MRI scans may provide doctors with an added tool to monitor NMOSD progression and let them anticipate future attacks even when patients aren’t having symptoms.
“We are pleased to see that the long-term Phase 3 pivotal trial data show that Uplizna effectively reduced subclinical MRI findings and NMOSD attacks while continuing to offer new learnings that help advance our understanding of the disease and improve patient care,” Patterson said.