Higher prevalence of NMOSD among non-white Americans: Study
Researchers reviewed data, ID'ing 115 seropositive patients
Written by |
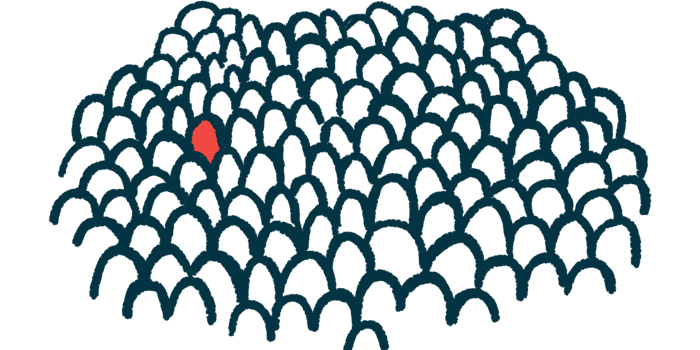
People who are Asian or Pacific Islander and Black are more likely to have neuromyelitis optica spectrum disorder (NMOSD) and test positive for self-reactive antibodies against aquaporin-4 (AQP4) than white people, a U.S.-based study suggests.
The prevalence of anti-AQP4 antibody-positive NMOSD was also higher among women and Hispanic people.
“Women and those identifying as Asian or Pacific Islander, Black, and Hispanic shoulder the highest burden of disease,” the researchers wrote. The study, “The epidemiology and clinical presentation of seropositive neuromyelitis optica spectrum disorder in a U.S. population,” was published in Annals of Clinical and Translational Neurology.
A progressive autoimmune disease, NMOSD is marked by inflammation in the spinal cord and the optic nerve, which sends and receives signals from the eye. People with NMOSD have periodic episodes of inflammation, separated by periods of remission. With each occurrence, symptoms such as vision problems, uncomfortable burning or tingling, and painful involuntary muscle contractions, tend to worsen.
The cause of NMOSD isn’t fully understood, but most patients test positive for self-reactive antibodies that target AQP4, a protein on the surface of nervous system support cells called astrocytes. The disease can be classified into two types based on the presence (seropositive) or absence (seronegative) of self-reactive AQP4 antibodies in blood serum.
Incidence, prevalence of NMOSD reviewed
Here, researchers looked at clinical data from a repository for the University of Colorado Health System and Children’s Hospital of Colorado, which includes information on about 7.3 million people. The goal was to use the dataset and determine the patterns, causes, and distribution of seropositive NMOSD patients. In total, 115 seropositive NMOSD patients were identified for the study.
The average yearly incidence of clinical onset, or the rate at which new NMOSD cases began to show noticeable symptoms, was 0.22 per 100,000 people over a year. This was “higher than most existing studies, including many European cohorts, and a cohort from Australia and New Zealand,” the researchers wrote.
Incidence measures the number of new cases of a condition that develop in a population in a specific time period. Prevalence is a proportion of a population over a given period with the condition being measured.
The differences in the incidence rate between men and women across different age groups, were also compared, with the findings showing the incidence of NMOSD was highest for women when they were between ages 55 and 64. NMOSD incidence was highest for men when they were older than 65.
Women were also more likely to have NMOSD. “The sex-adjusted prevalence ratio … of our cohort confirms the high burden of disease in women,” wrote the researchers, who also reviewed how common NMOSD was across racial and ethnic groups. “We captured detailed race and ethnicity data, further informing our understanding of the disease burden in key demographic groups, as well as addressing a gap in knowledge for both Hispanic U.S. populations and in Native American and Alaska Native populations.”
The rate of NMOSD was 17.72 per 100,000 for study participants who self-identified as Asian or Pacific Islander and 14.74 for participants who identified as Black. This was significantly higher than the prevalence of NMOSD for white people, at 3.45 per 100,000 people.
A small number of Native American and Alaska Native people were included. The prevalence was also high for this group — 7.18 per 100,000 people. The researchers said they were the first to provide information about the rate of NMOSD among Native Americans and Alaska Native people, but cautioned that their study was limited by the small sample size.
People who identified as Hispanic were also more likely to have NMOSD than those who identified as non-Hispanic.
In their analysis of initial clinical presentations associated with seropositive NMOSD, the researchers found the most common clinical presentation was transverse myelitis, or spinal cord inflammation, occurring in 45.21% of cases. Optic nerve inflammation, or optic neuritis, was the second most common clinical presentation and was unilateral in 68% of all the cases with the condition. About 10% of the patients presented with multiple areas of disease.
“In comparing to contemporary studies, this elevated incidence rate [relative to studies from Europe, Australia and New Zealand] appears to be driven largely by higher rates in those identifying as Hispanic, Asian, or Pacific Islander, and as Black,” the researchers wrote.