Pure oxygen therapy may reduce inflammation in NMOSD: Study
It could be especially beneficial for those with more overactive immune systems
Written by |
Add-on hyperbaric oxygen therapy (HBOT), which involves breathing pure oxygen at high pressure, may help reduce inflammation in people with neuromyelitis optica spectrum disorder (NMOSD), especially those with more overactive immune systems, a small study suggests.
“HBOT may help rebalance the immune system in NMOSD,” researchers wrote, noting that larger studies are needed to confirm the therapy’s long-term benefits.
The study, “Effect of hyperbaric oxygen therapy on peripheral blood inflammatory markers in patients with neuromyelitis optica spectrum disorder: a retrospective cohort study,” was published in Frontiers in Neurology.
HBOT aimed at increasing amount of oxygen dissolved in blood
In NMOSD, self-reactive antibodies attack healthy cells in the nervous system, causing inflammation in the spinal cord and the optic nerve, which connects the eyes to the brain. Because inflammation plays a key role in the disease, treatments that calm an overactive immune response may ease NMOSD symptoms and limit the disability that accumulates with each attack.
HBOT involves inhaling pure oxygen at pressures above normal atmospheric pressure to increase the amount of oxygen dissolved in the blood and delivered to tissues.
“Animal and clinical studies have shown that HBOT can achieve multiple effects, including anti-inflammatory, neuroprotective, and promoting injury repair,” the researchers wrote.
In multiple sclerosis, an NMOSD-related disease also marked by inflammation in the brain and spinal cord, “HBOT has shown potential in reducing neuroinflammation and improving functional outcomes,” the researchers wrote. “However, its impact on inflammatory response and immune balance in NMOSD patients [is] lacking.”
In this study, a team of researchers in China set out to evaluate whether biomarkers of inflammation, such as the neutrophil-to-lymphocyte ratio (NLR) and the platelet-to-lymphocyte ratio (PLR), change after HBOT in people with NMOSD.
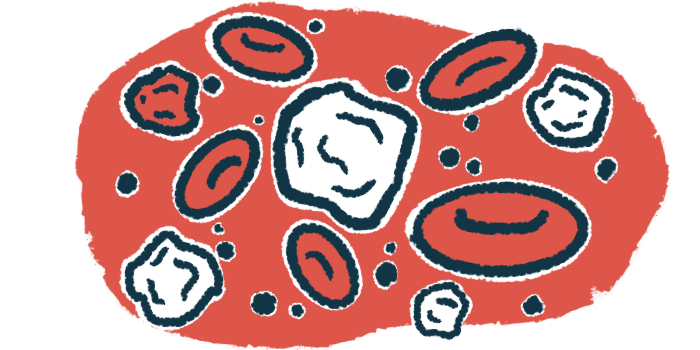
Platelets and neutrophils are the immune system’s first responders to infection or injury, triggering inflammation, while lymphocytes are mostly involved in slower and threat-specific immune responses. Lymphocytes also include specific subtypes involved in suppressing excessive immune responses.
Higher values in these ratios typically indicate body-wide inflammation.
“Previous studies have shown that higher NLR and PLR levels are closely associated with acute activity, relapse risk, and poor functional prognosis in NMOSD,” the researchers wrote.
HBOT group showed lower levels of inflammation biomarkers
The team retrospectively analyzed medical records of 36 adults diagnosed with NMOSD, of whom half received HBOT once daily, in addition to their standard treatment. Those in the HBOT group underwent a median of 12 sessions, corresponding to one course of treatment over four weeks.
All participants had been on a stable dose of immunosuppressants for at least two months before the study.
At the study’s start, there were no significant differences between the HBOT and non-HBOT groups in age, proportion of women, rate of immunosuppressant use, prednisone dosage, and NLR and PLR.
Data showed that after four weeks of treatment, the HBOT group showed a significantly lower NLR than the non-HBOT group (2.2 vs. 4.95), as well as a significantly lower PLR (170.1 vs. 220.3)
Patients who received add-on HBOT also showed a significantly higher lymphocyte count than those in the non-HBOT group.
When results were adjusted for any potential influencing factors, HBOT “remained significantly superior to the control group in reducing NLR … and PLR …, and in increasing lymphocyte count,” the team wrote.
This suggests that the benefit of HBOT was more prominent in patients with a higher pre-treatment inflammatory burden.
Also, patients with an NLR of 3 or higher at the study’s start, but not those with an NLR less than 3, showed a significant decrease in NLR following HBOT compared with the control group.
“This suggests that the benefit of HBOT was more prominent in patients with a higher pre-treatment inflammatory burden,” the researchers wrote. “This implies that treatment efficacy may be associated with the degree of [body-wide] immune activation.”
Over the four-week period, the Expanded Disability Status Scale, a standard measure of disability, did not change significantly in either group, and changes were comparable between the two groups.
No serious side effects occurred, and only mild, temporary ear pressure was reported in two patients (11.1%).
Overall, these findings suggest that add-on HBOT may rebalance the inflammatory response in NMOSD, especially in patients with more overactive immune systems. Still, “future studies should investigate the long-term efficacy and mechanisms of HBOT,” the researchers concluded.