Area postrema syndrome at NMOSD onset tied to relapse risk
Delayed diagnosis, treatment of APS can result in disease progression
Written by |
People having area postrema syndrome (APS), that is, uncontrollable nausea, vomiting, or hiccups, as the first symptom of neuromyelitis optica spectrum disorder (NMOSD) are more likely to relapse sooner and more frequently than those having another first symptom.
These are the main findings of a single-center study that retrospectively analyzed the natural course of NMOSD according to the first symptom experienced.
“Clinicians should pay attention to AP [area postrema] damage in NMOSD, as it indicates a potential risk of recurrence,” the researchers wrote in “Characteristics of recurrence in area postrema-onset NMO spectrum disorder-a retrospective cohort study,” which was published in BMC Neurology by researchers in China.
NMOSD is marked by inflammation in the spinal cord, called transverse myelitis, and the optic nerves (optic neuritis), which relay visual information from the eyes to the brain. As such, the main symptoms of NMOSD usually include weakness in the arms and legs, and vision problems.
While more rare, a sudden but long-lasting attack of nausea, vomiting, or hiccups, known as area postrema syndrome (APS), may also occur as the first symptom of NMOSD. This is due to damaging inflammation in a region called the area postrema on the brainstem, a stalk-like structure that sits at the base of the brain.
Area postrema syndrome in NMOSD
Because it’s rare and its symptoms can be mistaken for other diseases, having area postrema syndrome as a first NMOSD symptom “often leads to delayed diagnosis and treatment, resulting in disease progression,” wrote the researchers, who analyzed clinical data from 166 patients being followed for up to 20 years as part of an observational study (NCT04386018) to better understand how NMOSD progresses when it first manifests as APS.
All were positive for antibodies against aquaporin-4 (AQP4), the most common type of NMOSD-driving self-reactive antibodies.
Area postrema syndrome occurred as the first symptom in 24 patients (14.5%; APS group). In the other 142 patients (85.6%; non-APS group), the first manifestation was the result of an inflammatory attack elsewhere, most often the spinal cord (53.3%) and optic nerve (41.1%).
Compared with the non-APS group, the patients with APS at disease onset were significantly younger (34.6 vs. 42.3 years) and more likely to have at least two core inflammatory lesions from the start (33.3% vs. 9.2%).
The APS group scored lower on the Expanded Disability Status Scale (EDSS) both at the disease’s onset (0.7 vs. 4.2 points) and the last follow-up visit (1.9 vs. 3.3 points), indicating less severe disease disability.
The researchers studied the occurrence of relapses, which were defined as new or worsening symptoms that lasted at least a day, that were accompanied by new neurologic findings, occurring a month after a previous attack.
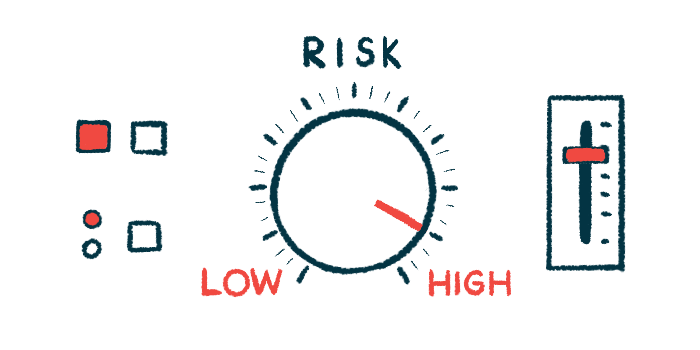
The average annualized recurrence rate, a measure of the number of relapses adjusted to a one-year time window, was significantly higher, by nearly twofold, in those with APS at onset relative to those without (0.4 vs. 0.19 relapses a year).
In those with APS at onset, the first relapse was significantly more likely to involve the brainstem (28.6% vs. 4.7%) and less likely to involve the optic nerve (10.7% vs. 41.1%).
Increased relapse risk
Having area postrema syndrome at onset was associated with an increased risk, by more than 2.5 times, of a first relapse, regardless of whether patients received immunotherapy or not after first episode.
This association was only statistically significant among the subgroup of nontreated patients. In these patients, APS at onset was associated with a two to three times higher risk of having the first relapse relative to optic neuritis or myelitis at onset.
These findings suggest inflammatory lesions in the area postrema may appear early in the disease or be more likely to occur in younger patients, who should “give them adequate attention and timely intervention,” the researchers wrote.
While the inflammatory lesions may initially bring less severe symptoms, a higher risk of recurrence may affect the disease course, the researchers said, adding. “early immunosuppressive therapy is necessary to reduce the risk of relapse and to avoid the accumulation of relapse-related disability.”