Inflammatory Neutrophils Resist Cell Death in AQP4 + NMOSD: Study
Findings highlight differences between NMOSD and MOGAD
Neutrophils, a set of immune cells, from people with aquaporin-4 (AQP4) antibody-positive neuromyelitis optica spectrum disorder (NMOSD) are resistant to certain forms of cell death, a study found.
NMOSD patients also had increased blood levels of molecules that might help neutrophils resist cell death pathways.
Similar findings weren’t observed in samples of myelin oligodendrocyte (MOG) protein-associated disease (MOGAD), a clinically similar, but distinct, condition.
These findings indicate a mechanism by which neutrophils may accumulate and contribute to inflammatory damage in NMOSD, and also corroborate “the notion that [AQP4-positive] NMOSD and MOGAD are pathogenetically different diseases,” the researchers wrote.
The study, “Impaired response of blood neutrophils to cell-death stimulus differentiates AQP4-IgG-seropositive NMOSD from MOGAD,” was published in the Journal of Inflammation.
NMOSD is a progressive autoimmune disease driven by self-reactive antibodies that target the central nervous system (CNS), comprising the brain and spinal cord. In most cases, these antibodies target AQP4, a protein present on nerve support cells called astrocytes.
For people without AQP4 antibodies, about 10-40% have MOG antibodies. While the symptoms of MOGAD and NMOSD are similar, they’re considered clinically distinct.
A growing body of literature suggests neutrophils may play an important role in NMOSD. The activation of these cells — first responders to infection or injury — is necessary to fight off foreign invaders, but that response must be shut off in order to resolve inflammation and prevent tissue damage. Consequently, neutrophils usually have a short lifespan in the bloodstream.
They are found to accumulate in active inflammatory brain and spinal cord lesions of NMOSD patients and animal models, where they are more active than in healthy people, however.
Exploring neutrophils’ resistance to cell death
In the study, researchers investigated whether neutrophils from NMOSD patients were resistant to the cell-death processes that normally regulate them, and examined these responses from people with AQP4-positive NMOSD, MOGAD, and healthy people recruited from institutes in Berlin between 2017-2021.
Blood samples were obtained from 28 NMOSD patients, 19 MOGAD patients, and 45 healthy controls. All the patients had been in remission for at least two months and most were using immunotherapies, most often rituximab.
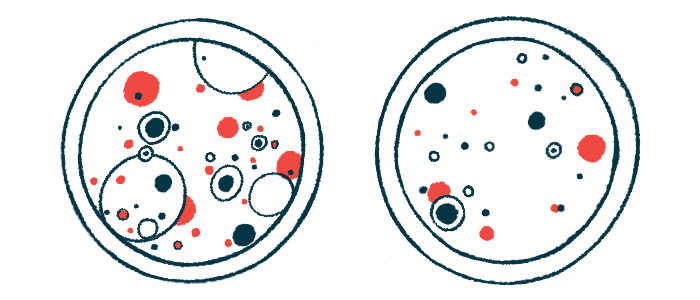
Neutrophils were isolated and grown in cell cultures where they were treated with a chemical called PMA to induce cell death. NMOSD neutrophils had a higher survival rate and lower death frequency in response to PMA compared with healthy controls, suggesting a resistance to cell death. This wasn’t seen in MOGAD patients’ cells.
NMOSD cells did enter an early stage of apoptosis, a type of programmed cell death, researchers observed. “Thus, although part of the AQP4 + NMOSD neutrophils enter the cell death pathway, they appear to be resistant to completing this process,” they wrote.
Similar trends were seen in a subset of cells from treatment-naive patients, “possibly excluding a potential effect of therapies on the observed impaired response of neutrophils to PMA,” the researchers wrote.
Neutrophils can undergo multiple types of cell death. In apoptosis, the cell is broken up into fragments and eaten up by other immune cells. In NETosis, cell components leak out to form a “trap” for pathogens outside of it, but the neutrophil dies in the process.
The apoptosis pathway appeared impaired after PMA exposure in the NMOSD cells, whereas NETosis did not, compared with healthy cells, experiments showed.
The researchers said further studies are needed “to understand whether apoptosis and NETosis are coexisting in our cell culture,” and whether these types of cell death might occur on different time courses not evaluated in the study.
In blood samples from the patients, circulating levels of cell-free DNA were higher in NMOSD patients than healthy controls and were correlated with levels of neurofilament light chain, a biomarker of nerve cell damage. This suggests that “both biomarkers could be combined to better assess disease progression,” the researchers wrote. Cell-free DNA are DNA fragments released into the bloodstream during cell death.
Levels of the anti-apoptotic molecule GM-CSF were also higher in NMOSD samples compared with controls, which may be at the root of these cells’ resistance to cell death, the researchers noted, adding the pro-apoptotic molecule IL-10 was also increased and should be investigated in future studies. IL-15, a molecule linked to neutrophil activation, was increased in both NMOSD and MOGAD.
“Taken together, our data show a different response to PMA in neutrophils from [AQP4-positive] NMOSD and MOGAD patients when compared to their corresponding [healthy controls],” the researchers wrote.
Prolonged neutrophil survival or delayed apoptosis has also been reported in other inflammatory diseases, including ANCA-associated vasculitis, rheumatoid arthritis, and cystic fibrosis, among others.
“An increased lifespan, accompanied by neutrophil accumulation, may contribute to the maintenance of a pro-inflammatory environment within the CNS,” they noted.