Diagnosis of NMOSD
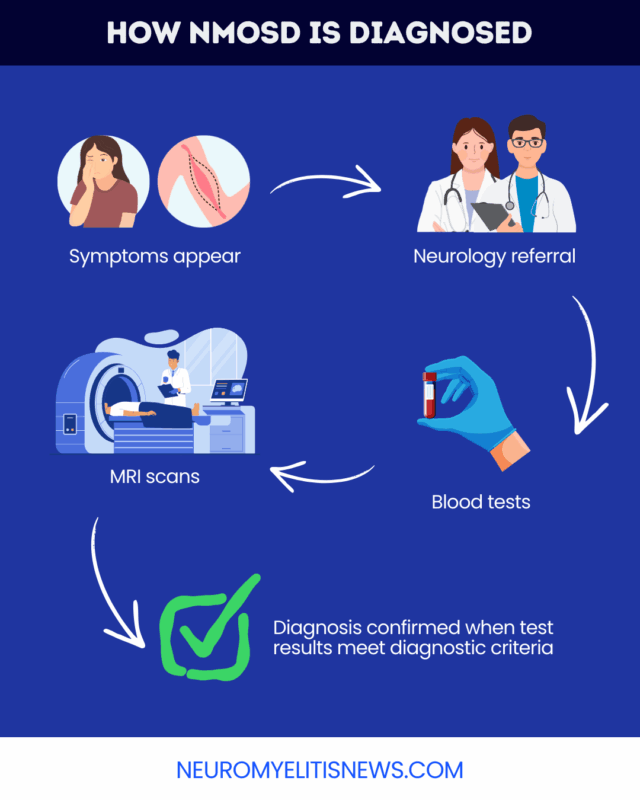
Reaching a diagnosis of neuromyelitis optica spectrum disorder (NMOSD), a rare autoimmune disease, involves clinical examinations, blood tests, and MRI scans. Collectively, these tests identify hallmarks of NMOSD and exclude other possible diagnoses.
NMOSD is caused by the immune system’s mistaken attacks against healthy parts of the nervous system, particularly the spinal cord and optic nerves, which transmit signals between the eyes and the brain. Self-reactive antibodies against the aquaporin-4 (AQP4) protein drive these attacks in most cases.
An accurate and prompt NMOSD diagnosis is important because it enables the start of treatments that can help slow disease progression and ease symptoms to allow the best possible quality of life.
When symptoms point to NMOSD
There are three groups of symptoms that most often lead clinicians to suspect NMOSD:
- optic neuritis: vision changes, or eye pain
- myelitis: nerve pain, muscle weakness, numbness, bladder, bowel, or sexual problems
- area postrema syndrome: nausea, vomiting, and hiccups
Optic neuritis is related to optic nerve damage, and myelitis to spinal cord damage. Area postrema syndrome affects an area of the brain called the brainstem. It is not as common as optic neuritis or myelitis, but is more specific for NMOSD.
Some of these symptoms, particularly those of optic neuritis and myelitis, resemble early signs of multiple sclerosis (MS), a more common neurodegenerative disease. Working with a specialist who understands how NMOSD is diagnosed can help reduce the chances of a misdiagnosis.
Diagnostic tests
There is no single test that can definitively diagnose NMOSD. After a thorough physical and neurological examination, a few different NMOSD diagnostic tests are needed to confirm the disease and rule out other possible diagnoses, including:
- blood tests: to look for NMOSD-causing antibodies
- MRI scans: to identify areas of nervous system damage
- lumbar punctures: to identify signs of inflammation or other disease signatures in the nervous system
Blood tests
An NMOSD blood test is recommended as the first evaluation. It is most accurate when performed during a period of active symptoms and before treatment has been initiated.
Most people with NMOSD have elevated anti-AQP4 antibodies in the blood, which are not usually seen in MS. A positive AQP4 antibody test result is thus strongly suggestive of NMOSD. However, it is still possible to have the disease with a negative result. Repeat testing and other evaluations are recommended for such individuals.
Blood tests are also used to rule out other conditions. For example, they can detect antibodies against the myelin oligodendrocyte glycoprotein (MOG), which are associated with a condition that can cause similar symptoms called MOG antibody-associated disease (MOGAD).
MRI scans
MRI scans allow clinicians to identify areas of inflammation and damage, or lesions, in the nervous system. NMOSD MRIs may evaluate the brain, optic nerve, and spinal cord, and are especially useful in individuals who test negative for AQP4-targeting antibodies, known as seronegative NMOSD.
MRI findings in NMOSD — including the location, shape, and size of the lesions — can help differentiate it from other neurological conditions. Some MRI findings that may particularly raise suspicion of NMOSD include:
- areas of long, continuous lesions on a spinal cord MRI
- lesions in the area postrema or nearby parts of the brainstem
While there is some overlap, the patterns of damage in MS tend to look different.
Lumbar puncture
A lumbar puncture, also called a spinal tap for NMOSD, isn’t always necessary, but is often recommended to help rule out other possible diagnoses.
During the procedure, a healthcare provider inserts a needle into the lower back to collect a sample of the cerebrospinal fluid (CSF), which circulates around the brain and spinal cord. The sample is analyzed in a lab to look for signs of immune activity, neurological damage, or antibodies that might suggest NMOSD, MS, or another condition.
Diagnostic criteria
International NMOSD diagnostic criteria outline six core clinical characteristics of the disorder:
- optic neuritis
- acute myelitis
- area postrema syndrome
- other acute brainstem syndromes
- symptoms and MRI findings suggestive of damage in a brain area called the diencephalon
- symptoms and MRI findings suggestive of damage in the largest part of the brain called the cerebrum
Because diencephalon and cerebrum symptoms are less specific to NMOSD than the other characteristics, clinicians need MRI confirmation that the damage looks typical of the disease.
The number of clinical characteristics needed to diagnose NMOSD depends on whether a person tests positive for AQP4-targeting antibodies:
- positive antibody test: one core characteristic
- negative antibody test or unknown antibody status: two core characteristics (occurring together or in separate attacks), with at least one being optic neuritis, myelitis, or area postrema syndrome, and NMOSD-typical MRI findings
Doctors must exclude other possible causes of symptoms and damage in all cases.
Conditions that can be confused with NMOSD
NMOSD can vary and overlap substantially with other neurological conditions, and NMOSD misdiagnosis is common. Conditions mistaken for NMOSD may include:
- MS and other inflammatory or autoimmune diseases, such as sarcoidosis, Behcet’s disease, and lupus
- MOGAD
- infectious diseases or cancer
- traumatic injuries to the spinal cord, brain, or optic nerve
MS and MOGAD are the diseases most commonly confused with NMOSD. A MOG antibody test can help rule out MOGAD, while differentiating between NMOSD and MS may involve a combination of blood, CSF, and MRI examinations.
Making these distinctions is vital because, despite overlapping clinical characteristics, treatment approaches differ between these conditions.
What happens after diagnosis
After an NMOSD diagnosis, individuals should work with their care team, including a neurologist with experience in the disease, to come up with an appropriate treatment plan.
Facing an NMOSD diagnosis can also lead to emotional and mental health challenges. Counseling and support groups can help patients and caregivers cope with the treatment process and adjust to life with NMOSD.
Neuromyelitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

