Causes of NMOSD
Neuromyelitis optica spectrum disorder (NMOSD) is a rare autoimmune disease that occurs when the immune system mistakenly attacks healthy parts of the nervous system. These attacks most often affect the optic nerves, which carry visual signals from the eyes to the brain, and the spinal cord, which relays messages between the brain and the rest of the body.
Self-reactive antibodies that target the aquaporin-4 (AQP4) protein appear to play a major role in autoimmune attacks on the optic nerve and spinal cord. However, the role of the immune system in NMOSD is complex, and researchers do not yet fully understand why the immune system begins to malfunction. A combination of genetic susceptibility and environmental factors is thought to be involved.
Several other neurological conditions can resemble NMOSD but require different treatment approaches. For this reason, understanding what causes NMOSD is essential for reaching an accurate diagnosis and starting appropriate treatment as early as possible.
Anti-AQP4 antibodies
Around 70%-80% of people with NMOSD have elevated blood levels of antibodies that target AQP4. This protein acts as a channel to regulate the flow of water in and out of nerve support cells called astrocytes, a process crucial to maintaining nervous system health.
Anti-AQP4 antibodies are believed to drive NMOSD by binding to the AQP4 protein and activating immune pathways that ultimately lead to astrocyte damage and cell death.
The resulting inflammation can also damage nearby nerve cells and oligodendrocytes — which are the cells that produce myelin, the protective coating around nerve fibers. Loss of oligodendrocytes and myelin leaves nerve cells susceptible to further harm.
One of the most common NMOSD misconceptions is that the disease is a subtype of multiple sclerosis (MS), a neurodegenerative disease also marked by myelin loss. However, NMOSD is now recognized as a clinically distinct disease. Because anti-AQP4 antibodies are typically not found in people with MS, testing for these antibodies plays a crucial role in confirming an accurate NMOSD diagnosis.
MOG antibodies and related conditions
Sometimes, a person with symptoms that resemble NMOSD tests negative for anti-AQP4 antibodies but positive for antibodies against another protein called myelin oligodendrocyte glycoprotein (MOG). These antibodies directly target oligodendrocytes and myelin, the cells and structures that protect nerve fibers.
Researchers once thought that anti-MOG antibodies might represent another cause of NMOSD. It is now recognized that their presence often signals a distinct disorder called MOG antibody-associated disease, or MOGAD.
While MOGAD and NMOSD can share similar symptoms, there are some important clinical differences between the two. Compared with AQP4 antibody-positive NMOSD, MOGAD:
- is less likely to involve repeated symptom episodes (relapses) or lead to permanent disability
- affects males and females more equally, whereas NMOSD is more common in women
- is more likely to occur in children
Seronegative NMOSD
If a person has at least two core clinical features of NMOSD but an NMOSD antibody test is negative for antibodies against AQP4 or MOG, they may be diagnosed with seronegative NMOSD.
The underlying seronegative NMOSD causes are not fully understood. Researchers suspect that other, as-yet-unidentified antibodies or immune factors may be involved.
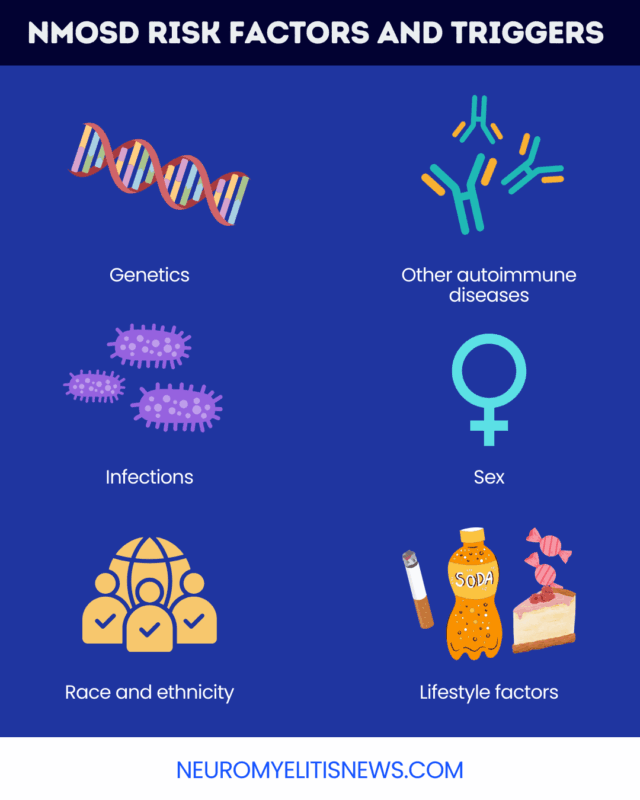
Genetic factors and NMOSD
NMOSD is not hereditary, meaning it is not generally passed down through families via specific genetic mutations. However, genetic factors can influence a person’s susceptibility to the disease.
Certain genetic variants are more common in people with NMOSD than in the general population. These variants may contribute to disease development by how the immune system functions.
Genetic factors may also help explain some of the other well-established risk factors for NMOSD, including:
- a personal or family history of other autoimmune conditions. Autoimmune diseases linked to NMOSD include lupus and Sjögren’s disease
- female sex, possibly reflecting interactions between hormones and immune-related genes
- race and ethnicity, with inherited genetic variants potentially contributing to why NMOSD disproportionately affects people of African and Asian descent
| Genetic risk | Genetic inheritance |
|---|---|
| Genetic mutations don’t directly cause the disease, but influence the chances it develops | Genetic mutations directly cause the disease |
| Can influence disease probability in unpredictable ways; may involve a combination of genetic variants inherited from both parents | Has a more well-defined effect on disease risk; biological parents have a predictable chance of passing mutations to children |
| Disease often occurs in the absence of a family history | There is often a family history of the disease |
| Genetic factors usually interact with a variety of environmental factors to influence disease risk | Environmental risk factors play a smaller role, if any |
Environmental triggers and risk factors
External or environmental factors can also affect the probability of developing NMOSD. In people who are already susceptible, certain events may trigger the first symptoms of the disease or cause a relapse.
In particular, studies have found links between certain viral or bacterial infections and NMOSD. These infections may activate the immune system in ways that trigger an NMOSD attack, although researchers do not yet fully understand the underlying mechanisms. Other factors, such as allergic reactions, injuries, surgeries, or hormonal changes, may also trigger NMOSD attacks.
Researchers have also examined a range of possible lifestyle and environmental NMOSD risk factors, including:
- vitamin D deficiency
- smoking
- high-sugar diet
However, evidence linking each of these factors to NMOSD is mixed and sometimes contradictory. More research is needed to fully understand the role of these factors in the development and progression of NMOSD.
Neuromyelitis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

