Rituximab Helps Ease Disability in Children With NMOSD, Study Finds
60% of children with inflammatory neurological disorders improved in study

Rituximab may be effective for improving functionality in children with neuromyelitis optica spectrum disorder (NMOSD) or other inflammatory neurological disorders, though more research is needed to identify optimal treatment regimens, a new study reports.
“Efficacy of [rituximab] in specific indications and good tolerance are confirmed in pediatric neurology. … Further study is needed to optimize dose regimen in adults and children,” researchers wrote.
The study, “Indications and safety of rituximab in pediatric neurology: a 10-year retrospective study,” was published in the journal Pediatric Neurology.
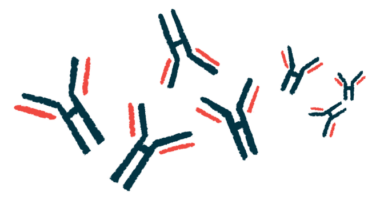
What is rituximab?
Rituximab is a monoclonal antibody that works by killing a type of immune cell called B-cells. First developed to treat blood cancers, the therapy is commonly used off-label for adults with a number of inflammatory neurological conditions including NMOSD and multiple sclerosis. There has been minimal research on the use of rituximab to treat inflammatory neurological disorders in children, however.
Here, researchers presented data for 77 children treated with rituximab at the Necker-Enfants Malades University Hospital, in France, between May 31, 2010, and May 31, 2020. Among these children, six had NMOSD, and the rest had other inflammatory diseases like myasthenia gravis, encephalitis, or opsoclonus-myoclonus syndrome.
In most of the patients (68%), rituximab was given as a second-line therapy after the patient had an inadequate response to initial treatment. Median time from disease onset to rituximab treatment was just under four months; most patients received rituximab within a year of symptoms first appearing.
Over 90% of patients received an initial treatment regimen with four weekly infusions of rituximab at a dose of 375 mg per square meter of body area. Most patients received an additional two weekly infusions afterwards.
Following standard procedures, prior to rituximab infusion all the patients were treated with antihistamines and other medications to prevent side effects like allergic reactions. Nearly all patients received infusions of antibodies after treatment, which can help reduce the risk of infection when the body lacks B-cells that are responsible for making antibodies.
As of the publication of the study, 63 of the 77 patients were no longer taking rituximab, the most common reason being clinical improvement or complete recovery in 60% of cases. Most other patients have switched to other treatments.
Over a median follow-up time of 3.5 years, six (8%) of the 77 children experienced side effects deemed related to rituximab treatment. Four had mild allergic reactions after the first infusion, manifesting as abdominal pain and/or hives, which was resolved by slowing or pausing the infusion; antihistamines were also needed for two patients.
Two patients experienced infection deemed related to a weakened immune system due to rituximab — one serious case of the fungal infection pneumocystis that required hospitalization, and one case of COVID-19 that resolved without specific treatment.
Among the patients with NMOSD and related conditions, the median score on the expanded disability status scale (EDSS) decreased from 6.5 to 1.5 following rituximab treatment, reflecting markedly better ability to function for the children. Clinician-reported disability severity improved following rituximab for all NMOSD patients.
“All 6 patients with NMO spectrum disorders in our cohort had a positive outcome, i.e. with an Expanded Disability Status Scale less than 5,” the researchers wrote. An EDSS score of at least 5 reflects disability that interferes with day-to-day activities.
In 45 of the children who underwent regular monitoring of B-cell counts, 42% had B-cell repopulation within about five months of rituximab treatment. Statistical analyses indicated that this type of B-cell recovery was more common in patients who’d had more recent treatment with preventive antibody infusions, or who’d received less than four rituximab infusions in the initial course.
Highlighting that this study is limited by its small size, single-center nature, and the inclusion of numerous different conditions, the researchers called for more research to optimize rituximab treatment for children with inflammatory neurological disorders.