Postpartum Women at Risk of NMOSD Onset, Rebound: Study
Immunotherapy during pregnancy reduced the risk of relapse fivefold
Written by |
Women are more likely to have neuromyelitis optica spectrum disorder (NMOSD) symptoms, or a rebound of symptoms, within three months after delivering a baby, a Chinese study found.
Women who didn’t receive immunotherapy during pregnancy and the postpartum period were more than five times as likely to have a rebound as those who did get immunotherapy, researchers also found.
“Immunotherapy during pregnancy and the postpartum period might be recommended to decrease the risk of pregnancy-related attacks,” the researchers wrote, noting that “larger-scale prospective studies are warranted to confirm our findings.”
The study, “Effects of pregnancy on neuromyelitis optica spectrum disorder and predictors of related attacks,” was published in Annals of Clinical and Translational Neurology.
NMOSD occurs when the immune system erroneously attacks cells in the nervous system. This leads to the loss of myelin, a fatty sheath around the nerve cells, and damage to the spinal cord and the optic nerves.
The disease can affect anyone, but it occurs more often in women than men. Its symptoms can be one-off or recurring, and can worsen quickly.
What sets off an attack of symptoms is unclear and can look different for every person, but women with NMOSD are more likely to have a relapse soon after they give birth or end a pregnancy.
NMOSD and pregnancy
To identify what triggers NMOSD in pregnancy or after delivery, a team of researchers drew on data from women who received a NMOSD diagnosis at a single hospital in China between September 2009 and September 2020. Their median age was 25.1, and 30 (26.8%) had other autoimmune diseases.
Of the 112 women who reported a pregnancy, 46 (41.1%) had their first NMOSD symptoms during pregnancy or within a year after they gave birth or ended their pregnancy.
The remaining 81 (72.3%) women had 155 pregnancies after the onset of NMOSD. More than half (51.6%) of these pregnancies resulted in abortion, whereas the remaining 75 pregnancies resulted in live births. Ten of these babies were born preterm.
The most common reason for an abortion was an unplanned pregnancy (60%), followed by fear of taking medications that might’ve been unsafe for the babies (15.8%). In nine cases (9.5%), the abortion was due to an attack of NMOSD during pregnancy.
“The absence of definitive evidence based on guidelines seemed to be the main reason for the high rate of abortions,” the researchers wrote.
In 15 (20%) of the 75 pregnancies that resulted in live births, the women had relapses during the year prior to getting pregnant. In nine (12%), relapses occurred during pregnancy. And in 42 (56%), relapses occurred a year after pregnancy. The median time to relapse in all 52 cases with relapses within a year after delivery was three months.
The annualized relapse rate, a measure of the average number of relapses in a year, was more than six times higher in the first three months after pregnancy than it was before pregnancy (1.44 vs. 0.23). In contrast, no difference was found comparing this rate during and before pregnancy.
The mean Expanded Disability Status Scale score also increased from 1.40 to 1.99 points a year after delivery and more than a third (34.7%) of pregnancies were linked to worse disability compared to before pregnancy.
Effect of immunotherapy
Women who got pregnant after they were diagnosed with NMOSD were receiving immunotherapy a year before their pregnancies in 32 (20.6%) of the cases. In 28 (18.1%) of the 155 pregnancies, women also received immunotherapy during pregnancy or the postpartum period.
Immunotherapy included oral glucocorticoids, oral tacrolimus, oral glucocorticoids plus azathioprine, or oral glucocorticoids plus mycophenolate mofetil (sold as CellCept).
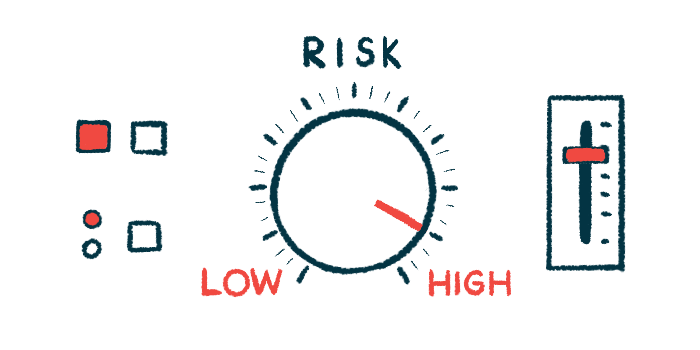
When the researchers looked for risk factors of a relapse in pregnant or postpartum women, they found that those whose disease activity increased a year before getting pregnant had 79% higher risk of a rebound.
Those who didn’t receive immunotherapy during pregnancy and in the postpartum period were 5.25 times as likely to have a rebound. This association was subsequently confirmed in a different analysis.
“Lack of immunotherapy during pregnancy and the postpartum period was an independent risk factor that predicted pregnancy-related attacks,” the researchers wrote. “Immunotherapy during pregnancy and the postpartum period may reduce the risk of relapse.”