Immune B-cells train T-cells to prevent NMOSD: Mouse study
Understanding immune mechanisms may help with prevention, treatment
Written by |
Under normal circumstances, immune B-cells train T-cells, another type of immune cell, on which targets not to attack, preventing the development of neuromyelitis optica spectrum disorder (NMOSD), according to a study in mice.
This training occurs in the thymus gland, a small organ behind the breastbone that works as a school for T-cells. While thymus cells were known to be involved in this learning process, this is the first time that B-cells were shown to also be implicated.
The findings imply that this training system must break down somehow in order for NMOSD to develop. Better understanding of these immune mechanisms may ultimately pave the way toward new ways to treat or prevent NMOSD and other autoimmune diseases.
“Looking further into the future, this interaction in the thymus might be exploited to treat existing autoimmune diseases in a very targeted manner,” Thomas Korn, MD, professor of experimental neuroimmunology and a senior author of the study at the Technical University of Munich in Germany and , said in a press release.
The study, “B cells orchestrate tolerance to the neuromyelitis optica autoantigen AQP4,” was published in Nature.
Cells spur each other to trigger an inflammatory attack
B-cells and T-cells are both essential for keeping the body safe from infections, but they also play central roles in autoimmune disorders like NMOSD. Both types of cells are equipped with special molecular receptors that allow the cell to recognize a specific target.
When the receptor engages its target, it triggers the cell to go on the attack. When B-cells and T-cells are both responding to the same target, the cells can spur each other on to trigger a powerful inflammatory attack, which is one of the main ways the body is able to rapidly mount immune responses to fend off infections.
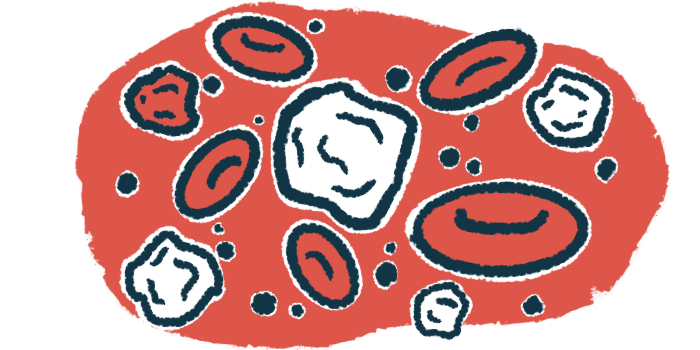
Since the receptors on T-cells control what the cells will recognize as a threat to be attacked, quality control systems have evolved to stop T-cells from making receptors that might accidentally recognize the body’s own tissue and trigger autoimmunity. This T-cell boot camp mainly takes place in the thymus.
Basically, T-cells made in the bone marrow are sent to the thymus, where thymus cells show the T-cells several proteins that are normally found in the body. Any T-cells that react to these healthy body proteins are destroyed, leaving only those that don’t react to the body’s own tissue to go out and patrol for threats.
B-cells also undergo a similar type of training, but in the bone marrow. It’s long been known that there are also B-cells in the thymus alongside T-cells, but exactly what they do there hasn’t been clear.
“The function of B cells in the thymus gland has been a mystery that has puzzled immunologists for many years,” Korn said.
NMOSD is characterized by an autoimmune attack that targets AQP4, a protein found mainly at the surface of neuron-supporting cells in the brain.
Now, Korn and colleagues demonstrated that B-cells in the thymus are essential for removing T-cells with receptors that could recognize this protein, and therefore launch an immune attack against it.
The researchers showed that healthy mice don’t have mature T-cells against AQP4, meaning that any T-cells with anti-AQP4 receptors were eliminated in the thymus before they could mature.
But in mice engineered so their B-cells could no longer make AQP4, the anti-AQP4 T-cells weren’t efficiently eliminated in the thymus, leading to an autoimmune attack targeting AQP4, similar to what’s seen in people with NMOSD.
“These data indicated that B cells contributed significantly to the purging of AQP4-specific T cells,” the researchers wrote.
This only happened when B-cells weren’t producing AQP4 — when thymus cells weren’t able to produce the protein but B-cells were, T-cells with anti-AQP4 receptors were eliminated as normal. This shows it’s the B-cells, not the thymus cells, that are needed to remove these abnormal T-cells.
Specific subset of thymic B-cells lead to destruction of those binding to AQP4
Further experiments showed that it’s only a specific subset of thymic B-cells, specifically those which have been activated through a cell surface receptor called CD40, that are able to present AQP4 to T-cells, leading to the destruction of those binding to AQP4.
Further evidence suggested that “CD40-licensed thymic B cells might be essential negative selectors not only for AQP4 but for a set of disease-relevant [molecules] in a variety of tissues,” the researchers wrote.
“We suspect that this previously unknown process has evolved particularly to prevent dangerous interactions between [self-reactive] T and B cells in the lymph nodes and spleen, the so-called peripheral immune compartment,” says Ludger Klein, PhD, another study co-senior author at Ludwig Maximilian University of Munich and a Professor of Immunology at Ludwig Maximilian University of Munich’s Biomedical Center.
Such encounters could lead to a sudden large-scale autoimmune attack.
“We assume that problems with the training of T cells by the B cells in the thymus can cause other autoimmune diseases as well,” Korn said. “After all, the B cells in the thymus present a whole range of the body’s own proteins. The corresponding interactions must be investigated in further studies.”