Developing NMOSD when older linked to worse symptoms: Study
Relapse patterns correlated with age at NMOSD onset, sex, treatment
Written by |

People who develop neuromyelitis optica spectrum disorder (NMOSD) at an older age are more likely to experience spinal cord inflammation and less likely to have eye nerve involvement, not only in the first attack but also in subsequent relapses, a study has found.
In addition, data show “different relapse patterns in patients with different onset ages, sexes, and treatment statuses.”
Before treatment with immunosuppressants, relapse risk increased in women who were older at disease onset, and was higher in men who were in the youngest and oldest age groups of disease onset.
After treatment, however, these trends changed for both sexes. Men and women showed a lower relapse risk when they developed NMOSD at older ages, “indicating a better response to [immunosuppressants] in these patients,” researchers noted.
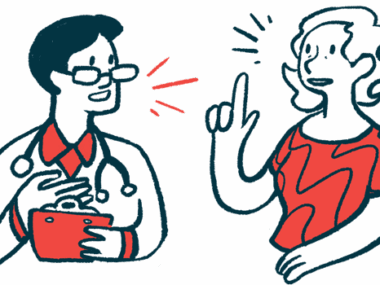
Understanding relapse patterns could help doctors better manage the disease
Understanding how age and sex may influence relapse patterns in NMOSD could help doctors tailor treatment plans and better manage the disease to prevent future relapses, researchers wrote.
The study, “Patterns of neuromyelitis optica spectrum disorder attacks in different age groups and sexes depending on the status of immunosuppressive therapy: A retrospective cohort study,” was published in the European Journal of Neurology.
NMOSD is characterized by damaging inflammation in the spinal cord (transverse myelitis) and optic nerves (optic neuritis). What exactly causes NMOSD is unclear, but self-reactive antibodies against the AQP4 protein are known to contribute to its onset.
The most common symptoms of NMOSD include weakness in the arms and legs, and eye pain and vision loss.
Patients often experience disease relapses, which are associated with accumulating, permanent disability. While “it is of vital importance to prevent relapses,” the researchers wrote, what may place patients at risk for a relapse is incompletely understood.
Some associations between age at disease onset, sex, and NMOSD relapses have been reported, but with some inconsistencies. In addition, “most previous studies have focused on patients who have received maintenance therapy, while the natural history of the disease in patients has been less studied,” the researchers wrote.
Study in China looked at natural NMOSD progression, relapses with treatment
To know more, researchers in China looked at how AQP4-related NMOSD progresses naturally in different age and sex groups, and how relapse patterns change with standard immunosuppressive treatment.
The study included 533 patients who experienced 1,394 attacks (861 relapses) before immunosuppressive treatment and 753 relapses after therapy. A relapse was defined as a worsening of symptoms over 24 hours, occurring 30 days after a prior attack or a new lesion on MRI.
Results showed more than half of the patients (60%) experienced transverse myelitis in the first attack, while more than one-third (39%) experienced optic neuritis instead.
The proportion of patients showing transverse myelitis as the first sign increased with age, from 49% in the youngest age group (18-29 years) to 68% in those 50 years and older. An opposite trend was observed for optic neuritis, with rates decreasing from 51% in the youngest age group to 35% in the oldest group.
There were no differences found in first attack presentation between men and women.
Similar findings were observed for the natural history analysis, before patients received immunosuppressive treatment. In addition, in this group of patients, older age at onset was associated with higher scores on the Expanded Disability Status Scale, indicating greater disability, both in the first attack and four subsequent relapses. Disability scores did not differ between men and women.
Relapse rates differed significantly between sexes
Before immunosuppressive treatment, patients who were older when they developed NMOSD showed a higher annualized relapse rate (ARR) compared with those in the youngest age group. Relapse rates were significantly higher in men than in women.
Also, “in different sexes, the correlation between age at onset and risk of relapse was completely different,” the team wrote.
The risk of relapse increased with older age of onset for women, while for men, this association took on a U-shape, meaning that men younger than 30 and those 50 and older at disease onset were at an increased risk of relapse.
After immunosuppressive treatment, “the ARR significantly decreased among age groups and sexes, and no difference in ARR was found among those groups,” the researchers wrote.
Moreover, the relationship between onset age and risk of relapse took on an inverted U-shape for women, with the highest risk of relapse seen in those ages 30 to 39 and the lowest after 50 years. For men, the risk of relapse decreased with older age at onset.
“The presentation of NMOSD attacks was related to age at onset, and relapse patterns were associated with age at onset, sex, and treatment,” the researchers wrote, adding that future large studies following patients over time “are needed to investigate the features of relapse with respect to age and sex.”