Anti-AQP4 antibodies linked to relapses, visual disability: Study
Relapses more severe in those with high levels even after treatment
Written by |
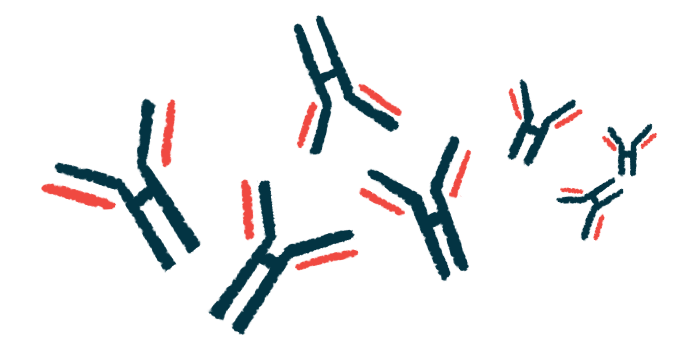
Higher levels of self-reactive antibodies against aquaporin-4 protein (AQP4), which drives neuroinflammation in most cases of neuromyelitis optica spectrum disorder (NMOSD), correlate with more severe relapses and visual disability, according to a large study.
Even after treatment with immunosuppressive agents, patients with high anti-AQP4 antibodies experienced more severe relapses.
Researchers suggested that anti-AQP4 levels may be a predictive biomarker in NMOSD. Their study, “Correlation between severe attacks and serum aquaporin-4 antibody titer in neuromyelitis optica spectrum disorder,” was published in the Journal of Neurology.
NMOSD is a rare inflammatory disease that primarily affects the spinal cord and optic nerves, those that transmit signals between the eyes and brain. This can lead to vision and/or movement problems. Typically, episodes of inflammation, or relapses, reoccur periodically, separated by periods of remission.
Most NMOSD patients have elevated levels of self-reactive antibodies that target AQP4, a protein found on nervous system support cells called astrocytes. Clinical observations suggest that patients who test positive for anti-AQP4 antibodies (AQP4-Abs) tend to experience more severe disease than those who test negative. However, it remains unclear whether the blood levels of these antibodies, referred to as titers, among those who test positive, are associated with the severity and frequency of relapses.
Comparing antibody levels with clinical data
Researchers at West China Hospital compared the levels of AQP4-Abs in 546 NMOSD patients (492 females and 54 males) with clinical data.
Among the participants, 155 (28.4%) had vision problems, 105 (19.2%) had motor disabilities, 71 (13%) had connective tissue diseases, and 44 had died (8.1%). Nearly all patients (85.5%) experienced a disease relapse.
AQP4-Abs were detected in 479 patients before treatment and in 67 patients after immunosuppressive therapy. Based on test results, patients were classified into two groups: high titer and low titer. There were no significant differences between the two groups regarding age at onset, sex, disease duration, co-existing connective tissue diseases, disease severity at onset, or mortality.
Results showed that patients with high AQP4-Ab titers had a significantly higher annual recurrence (relapse) rate than those in the low-titer group. High-titer patients also experienced more frequent attacks of severe optical nerve inflammation, called optic neuritis (ON), a higher total number of ON attacks, and a greater number of severe ON attacks.
AQP4-Ab titers were not related to the total number of severe spinal cord inflammatory attacks.
More patients in the high-titer group (21.9%) underwent immunosuppressive therapy with off-label rituximab (sold as Rituxan, among others) than in the low-titer group (7.2%).
Antibodies as potential outcome marker
Without immunosuppressive agents, there were 1,674 attacks. Of those, 682 were severe, including 376 severe ON attacks. Patients with elevated AQP4-Ab titers experienced a significantly higher number of severe attacks than those with low titers (49.1% vs. 36.2%), as well as severe ON attacks (64.2% vs. 49.0%).
Even after preventive maintenance therapy with rituximab and other standard treatments such as mycophenolate mofetil (Cellcept) and azathioprine, more people in the high-titer group experienced severe relapses (33.1% vs. 16.9%). Relapse-free rates were higher in the low-titer group (60.9% vs. 45.8% in the high-titer group).
While the high-titer group had more patients with vision problems (37.4% vs. 23.7% in the low-titer group), the levels of AQP4-Ab were not related to motor disability, disease severity, or mortality.
Consistent with these findings, those with elevated titers of AQP4-Ab had a significantly higher risk of visual disability than those with low titers. In contrast, time from NMOSD onset to motor disability or death did not show a significant difference between the two groups.
“Our findings highlight that the AQP4 titer exhibited an association with severe ON activity and an unfavorable visual prognosis in patients with NMOSD,” the researchers wrote. “This suggests the AQP4 titer may be a potential prognostic [outcome] marker in NMOSD.”